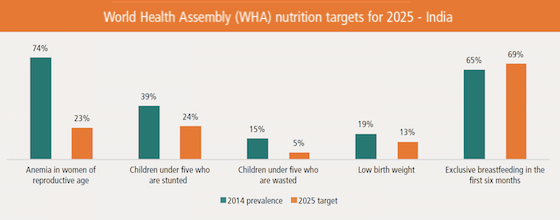
 The prevalence of nutritional outcomes such as stunting, anemia, wasting and low birth weight is persistently high in India. In 2012, India committed to achieving the six World Health Assembly (WHA) targets for nutrition. However, data on the prevalence of undernutrition shows that substantial improvements are required across all states, if India is to meet its WHA commitment by 2025. Thus, financial resources for nutrition need to be prioritized, expanded and well-utilized to deliver fully for nutrition in the coming decade.
The prevalence of nutritional outcomes such as stunting, anemia, wasting and low birth weight is persistently high in India. In 2012, India committed to achieving the six World Health Assembly (WHA) targets for nutrition. However, data on the prevalence of undernutrition shows that substantial improvements are required across all states, if India is to meet its WHA commitment by 2025. Thus, financial resources for nutrition need to be prioritized, expanded and well-utilized to deliver fully for nutrition in the coming decade.
National nutrition and health programmes in India– namely the Integrated Child Development Services (ICDS) and the National Rural Health Mission (NRHM)– are largely designed to provide evidence-based nutrition-specific interventions, but intervention coverage is low, likely due to a combination of implementation challenges, capacity and financing gaps. In previous work (Menon, McDonald and Chakrabarti, 2016), we estimated national and subnational costs of delivering recommended nutrition-specific interventions. In this new Policy Note, we’ve updated our previous cost estimates by projecting target population figures to 2017 using more recent undernutrition prevalence estimates, adding estimated costs for newly introduced and nationally mandated nutrition interventions–calcium supplementation and deworming for pregnant and lactating women. Together with Accountability Initiative, we also conducted an expenditure analyses using available data on nutrition-relevant government budget data.
The key takeaways from our study are:
- Across central and state budgets, India would need to consider investing INR 43,000 crore annually to fully finance the delivery of a core set of nutrition interventions, at scale. The estimates yield a thumb rule of about INR 9400 per year per child (0–24 months) for all interventions covered in the national policy framework.
- Where finances are limited, it would be wise for states to have flexibility to prioritize from a basket of interventions depending on their specific nutritional challenges, coverage gaps in interventions and implementation capability.
- States should rapidly scale-up low-cost interventions to take advantage of high benefit-cost ratios. These include interventions such as counseling for breastfeeding, iron-folic acid supplements for pregnant women, vitamin A supplementation, deworming and insecticide-treated nets for pregnant women in malaria-endemic areas,.
- Central and state governments should regularly track and monitor investments in nutrition, to allow for prioritization, planning and informed decision-making on allocations and expenditures by key actors.
- More research is needed to derive better estimates of unit costs of interventions.
India needs to invest strongly in nutrition in the coming decade, not just because of the global commitments or the high-value investment that nutrition spending is, but because India’s population has a right to the better life chances that come with better early life nutrition.
Click here to access the Policy Note